Robert Winston has slept through flood sirens, earthquakes, tornadoes and even an emergency plane landing.
Now, at age 88, Winston’s continued ability to sleep well makes him an exception among senior citizens.
Pitt psychiatry researchers Colleen McClung and Etienne Sibille studied the genes from post-mortem brain samples from 146 sudden-death adult subjects. Their findings, published in the Proceedings of the National Academy of Sciences on Dec. 21, 2015, indicated that the genes responsible for a person’s sleep-wake cycle change as people age, a finding Winston embodies.
Winston, a resident of Providence Point, a senior living community in Scott Township, said that he now wakes up multiple times a night to use the restroom and sleeps an average of an hour and a half longer than when he was younger.
“I’ve been very lucky, and I’m unique for my age, I’m aware of that. I talk to a lot of my contemporaries, those that are still with us, and they have a very different story to tell,” Winston said. “They need more sleep, [and] they have more difficulty getting it.”
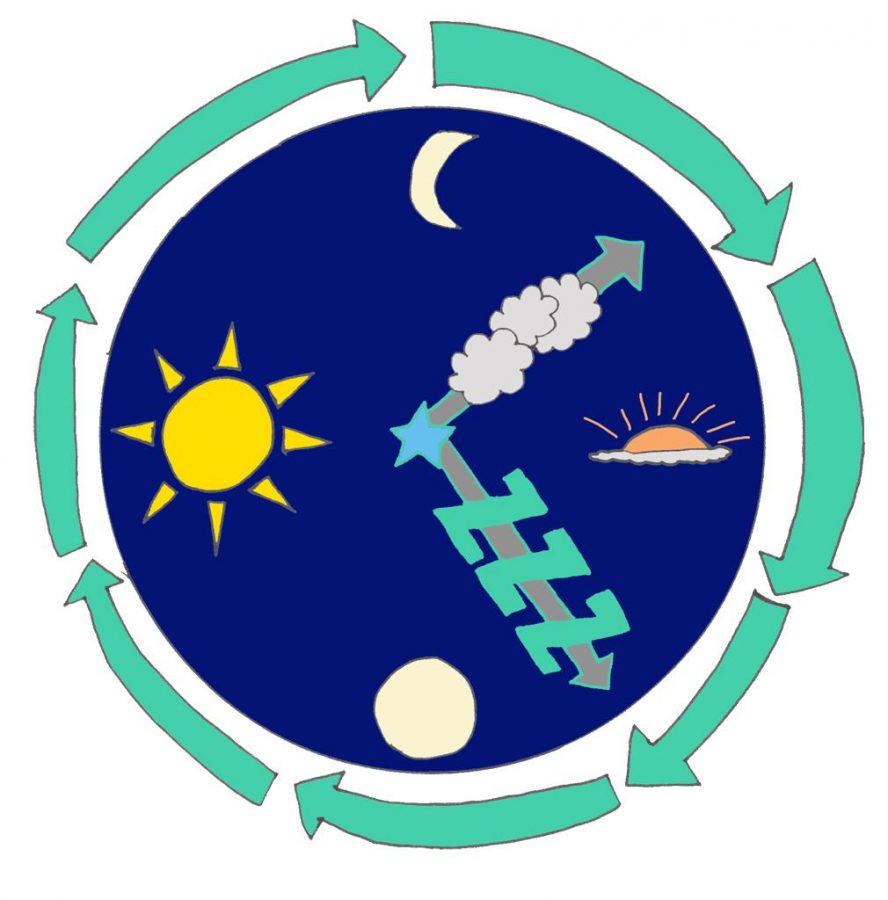
The “core clock” genes, which control a person’s circadian rhythm, the daily biological pattern that dictates sleepiness and alterness, had predictable patterns of expression throughout the day for people under 40, but became less rhythmic and often shifted earlier in the day for people above the age of 60.
“What was surprising was that we found another set of genes that actually gained rhythmicity in older people,” McClung, an associate professor of psychiatry at Pitt, said. “[This] suggested there might be a compensatory clock that kicks in, some maybe backup mechanism that’s trying to keep the rhythms going when you get older.”
According to the study, further research may lead to treatment development for illnesses that come with old age, such as Alzheimer’s and dementia.
Since other psychiatric illnesses unrelated to age are also associated with changes in daily rhythms, doctors and researchers could use treatments aimed at regulating the circadian rhythm in a wide variety of patients, such as those suffering from bipolar disorder and depression.
“There are many neuropsychiatric disorders that are characterized by change in daily life, change in rhythm,” Sibille, previously a professor of psychiatry at Pitt and currently a professor at the University of Toronto, said. “This study could tell us what genes are important targets.”
The research also yielded one major unexpected result: older subjects possess an unusual set of genes that don’t display rhythmic daily patterns until later in life. McClung and Sibille said this set of suddenly rhythmic genes may indicate a “backup clock” which maintains the circadian rhythm in older people, though they haven’t yet researched this hypothesis.
The increasingly rhythmic behavior of the unusual set of genes may be necessary for the brain to remain healthy, Sibille said.
“We’ve shown that 10-15 percent of the genes in the brain change with age, and these are not necessarily negative,” Sibille said. “They represent constant change with the brain to maintain function.”
The changing set of genes may help explain the continued regular patterns of exceptions, such as Winston. In most people, though, the possible backup clock does not make up for the loss of rhythm in the other major circadian genes.
As anecdotal evidence of the atypical sleep-wake cycles of senior citizens, McClung pointed to the early bird restaurant specials. Early bird specials typically cater toward an older audience, which supports McClung and Sibille’s findings that older people wake up and go to sleep earlier in the day.
Fabiana Cheistwer, the wellness director at Providence Point, said her facility offers dinner to residents around 5 p.m. as a result.
“Some [of the residents] might be in bed by 8 or 9,” Cheistwer said. “When I have an evening program, I need to be done between 8:30 and 9, because I have usually 10 to 20 percent of the [participants] fall asleep.”
Winston said he now goes to bed between 9:30 and 10 p.m., whereas he used to go to bed at 11 p.m., and still wakes up at the same time he used to.
“As you get older, you sleep more hours,” Winston said. “At least you try to sleep more hours, and I do. I sleep a good nine hours [a night].”
For some patients, evening brings more than just earlier sleep. Dementia patients with a condition called sundowning become increasingly disoriented and distressed during the evening hours, sometimes “almost psychotic,” according to McClung. A failure of the backup clock in the brain may partially cause this condition.
“We would suspect that people who have sundowning, not only are they losing rhythm in the core clock genes, but they’re probably not gaining rhythms in these other genes,” McClung said.
Since McClung and Sibille’s study did not analyze the brains of patients with dementia, Alzheimer’s or any other neurodegenerative condition, McClung said she hopes to continue research in this direction to determine whether theloss of circadian rhythm could evoke sundowning.
Potential treatments could include drugs that target the rhythmic genes identified in this study, in order to promote and maintain rhythmicity in individuals who display a lack of normal rhythms.
There are non-pharmaceutical treatment options as well, such as Interpersonal and Social Rhythm Therapy, a therapy requiring patients to maintain a strict pattern of sleep and daily activities.
“[IPSRT] is very beneficial for people with bipolar disorder, and it can help prevent mood episodes from happening,” McClung said. “It could be the same with Alzheimer’s and Parkinson’s — that if you can stabilize this circadian system, you might at least be able to delay the onset of it and help them have a little greater functioning for a longer time.”
McClung’s lab plans on continuing this research by looking at the effect of gene manipulation in mice, with the hope of someday applying their findings to human patients.
“We feel very strongly that if you can have treatments that stabilize and amplify circadian rhythms, that this is going to be beneficial for a whole host of diseases, including neurodegenerative disease, psychiatric disease, even cancer [and] diabetes,” McClung said. “It’s really becoming apparent that changes to circadian rhythms are fundamentally bad for you.”