EDITORIAL – Donor policy to go under the knife
April 3, 2007
In a move that has upset some doctors and ethicists, state legislatures across the United… In a move that has upset some doctors and ethicists, state legislatures across the United States are revising legislation addressing organ donation in order to help to meet the growing demand for kidneys, livers and other body parts.
Legislatures in Arkansas, Indiana, Iowa and New Mexico have now joined Virginia, Idaho, Utah and South Dakota in passing such legislation. At least 17 other states, as well as the District of Columbia and the U.S. Virgin Islands, are considering the legislation, according to a Washington Post report.
The legislation would make it clear that checking the box to become an organ donor at the driver’s license center is a lasting decision, one that cannot be revoked by a family member once a person has died. It will also expand the list of people who can consent to a brain dead patient becoming a donor.
This legislation would, in a way, make the decision to become an organ donor like a binding legal agreement. While the personal decision could always be made to retract one’s organ donor status, once a person dies, his wishes must be respected – as they should be.
Allowing gaps in the enforcement of organ-donor status can create situations in which family members completely monopolize a person’s health care decisions, with no regard for what he or she wanted in the first place. People choose to become organ donors in rational and thoughtful states of mind which can vary wildly from the emotionally heightened state of a family that has just lost a loved one.
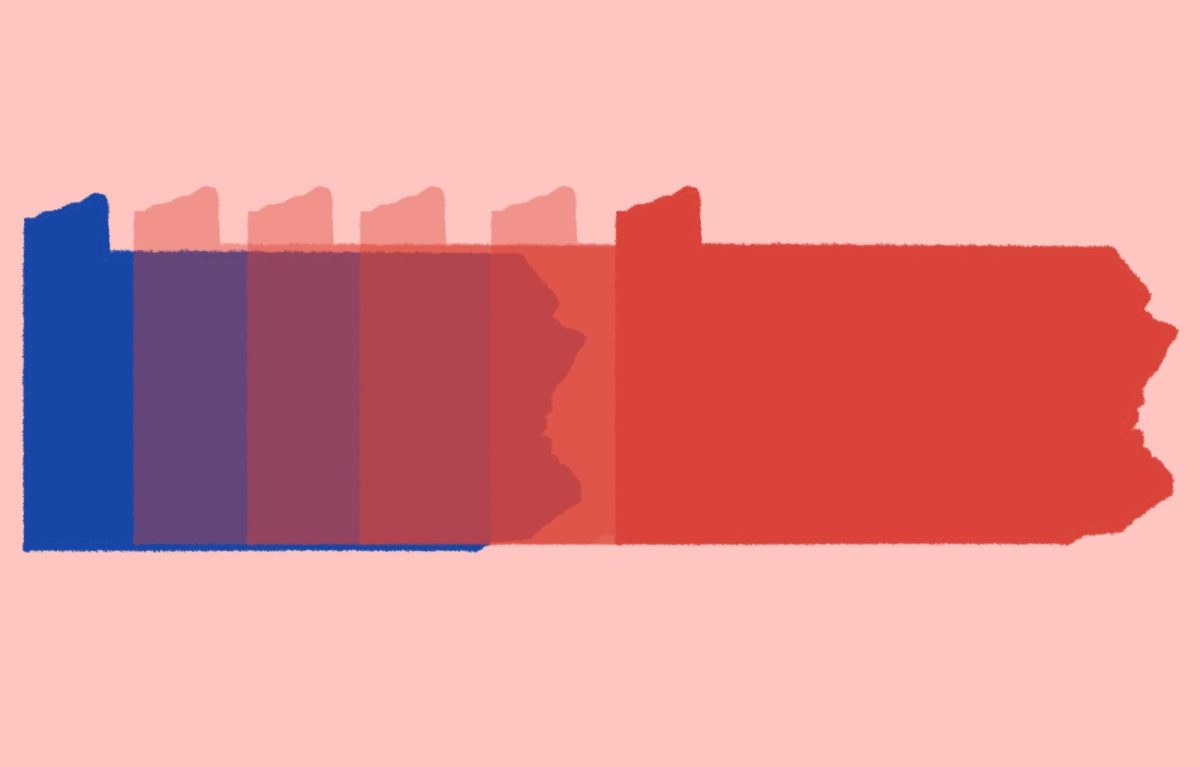
One side effect that does arise from forbidding family members or close relations to weigh in on organ donation is the question of which organs can be donated. Although in some states organ donors are given the choice of which body parts they would allow to be donated, other states, including Pennsylvania, offer no such option. States that pass the new legislation that do not already offer this type of option should consider adding it to their driver’s licenses.
One controversial part of this legislation deals with unconscious patients who have signed donor cards but also keep “living wills” or other documents specifying that they do not want a ventilator or medical care to keep them alive, which is sometimes necessary to maintain organ viability before a transplant. Under the legislation, organ donor cards will take precedent over the living will.
Ethicists and doctors worry that this part of the legislation is grounded on a false assumption that all people value donating their organs over avoiding living off of a respirator at the end of their lives.
In general, though, most people dictate through living wills to be taken off of respirators to prevent prolonged “vegetable-like” living. Organ donors would only be kept on a respirator for a short amount of time, a sacrifice that most donors would probably be willing to make to ensure that their organs were going to be transplanted to a grateful recipient.
But for those organ donors who strongly object to remaining on a respirator once their time has passed, it should be their responsibility to specify this wish in a living will.
The choice to become an organ donor is a personal decision that should not be infringed upon by any other family member or personal relation. This legislation is an important step in protecting the rights of organ donors and working to alleviate the chronic shortage of organs in the United States.