Pitt researchers find COVID-19 breakthrough in llama nanobodies
In a press conference Thursday afternoon, Pitt’s Dr. Yi Shi and Dr. Paul Duprex discussed the potential of nanobodies isolated from Wally the llama’s blood as a therapeutic treatment for COVID-19.
November 6, 2020
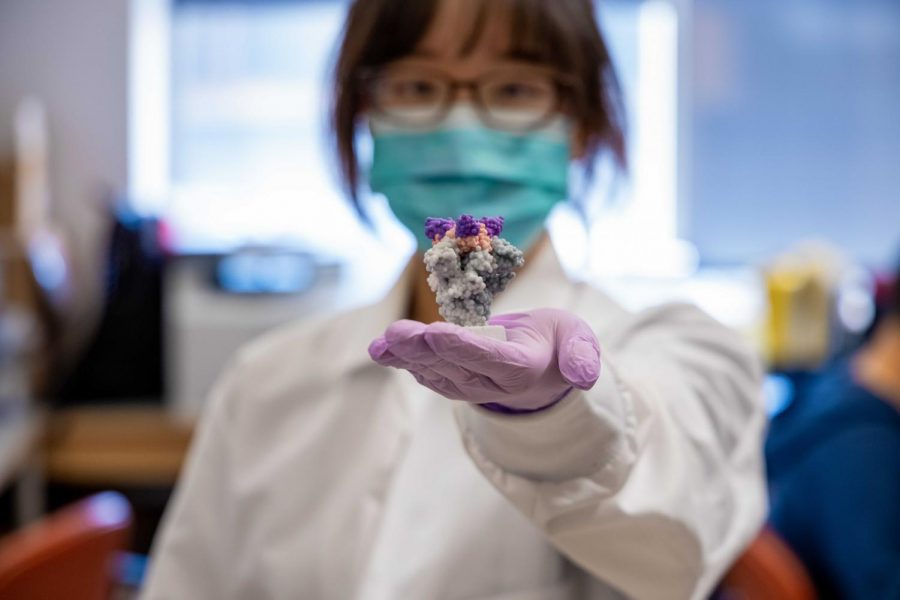
Yi Shi is using antibodies from an unconventional source to develop a COVID-19 treatment — Wally the llama.
Shi, an assistant professor of cell biology, and Paul Duprex, director of the Center for Vaccine Research, discussed using nanobodies isolated from Wally’s blood as a potential coronavirus treatment in a Thursday afternoon press conference. Nanobodies are small antibody fragments developed for therapeutic use. Llamas’ nanobodies are more potent and stable than the antibodies humans produce.
Shi’s research, published in “Science” Thursday in collaboration with Pitt’s Cheng Zhang and Hebrew University of Jerusalem’s Dina Schneidman-Duhovny, found these nanobodies have the potential to directly attack the SARS-CoV-2 spike protein. The virus SARS-CoV-2 causes COVID-19.
Duprex said the lab mixed a miniscule amount of the nanobodies with the live virus and added a few drops of that solution to a plate of cells. After a couple days, staff measured how well those nanobodies neutralized the virus and how many cells survived. Duprex said the results so far have been “promising.”
“Just a miniscule fraction of the nanobodies could neutralize enough SARS-CoV-2 to protect millions of cells,” Duprex said. “It is so much more effective than many of the other antibodies and all nanobodies identified to date.”
The results were so encouraging that “Science” — one of the world’s top academic journals — finalized the manuscript for rapid publication. Allison Hydzik, UPMC’s public relations director, said the news was “too important to sit on.”
Duprex said pre-clinical trials could move very quickly, in part due to the nanobodies’ key characteristics, such as its small size and reproducibility. But Duprex said a clinical trial is still far off.
“[The nanobodies] can be bulked up rather quickly — you can make it effectively and quite a large amount of it in standard bacterial systems,” Duprex said. “Being able to ramp up production — one of the big problems with vaccines — is really not such a big issue with these nanobodies.”
Shi added that the nanobodies also prevent SARS-CoV-2 from binding to human receptors.
“In this particular case, the nanobodies sitting on top of the virus will block the virus spike from opening to bind to the human receptors,” Shi said. “That means we can link several of the COVID nanobodies that we developed together like a Swiss Army knife, so that if the virus mutates to escape one nanobody, another will be there to keep it in check.”
Due to their smaller size, Shi said nanobodies are also a better option because they can be more easily delivered compared to the antibodies humans produce. Shi said it is possible that the nanobodies could be delivered by nasal spray rather than the conventional intravenous injection.
“They’re extremely potent and stable, which could be used for therapeutics,” Shi said. “Compared to the antibodies that usually require intravenous injection, [llama] nanobodies allow the possibility of direct inhalation, which makes direct delivery of the nanobody to the major infected organ, the lung, [possible].”
Shi added that the nanobodies can be freeze-dried for shipping and storage or kept at room temperature for six months, which will further aid drug development. Shi said this could dramatically drive down manufacturing costs and increase public access to COVID-19 treatment.
The road to this treatment has been long. Shi said his lab has been developing technology that helps target nanobodies of interest for three years using mass spectrometry. After the COVID-19 pandemic started, Shi’s lab used the technology to find some of the most potent nanobodies that could neutralize the virus in three months.
Shi’s lab drew Wally’s blood and isolated potent neutralizing antibodies 50 to 55 days after Wally was injected with the virus spike protein. Shi said even though Wally’s antibodies were necessary to produce the treatment, the lab won’t use any more llamas.

“As long as we get the [amino acid] sequence, we can produce quickly recombinant protein from these microbes, so we don’t need the llama any longer,” Shi said. “The key is actually the amino acid sequences from the nanobodies.”
To test its efficacy, Shi’s lab collaborated with the Center for Vaccine Research, which was among the first in the nation to receive live samples of SARS-CoV-2 directly from the Centers for Disease Control and Prevention in February. Duprex, co-author of the paper, said he was excited to work with Shi.
“What’s really nice about the Center for Vaccine Research is we have great neighbors, and Dr. Shi is one of those neighbors,” Duprex said. “Whenever he needed to test how well his antibodies worked, how well they faced off against SARS-CoV-2, he naturally talked to us as his neighborly virologists.”
Duprex said he and Shi will continue to work together on the scientific breakthrough that has the potential to be a therapy for COVID-19.
“We see each other and we chat about science often,” Duprex said. “And that’s how science works, communicating and talking about new ideas.”