Pitt researchers developing virus-repellent textiles
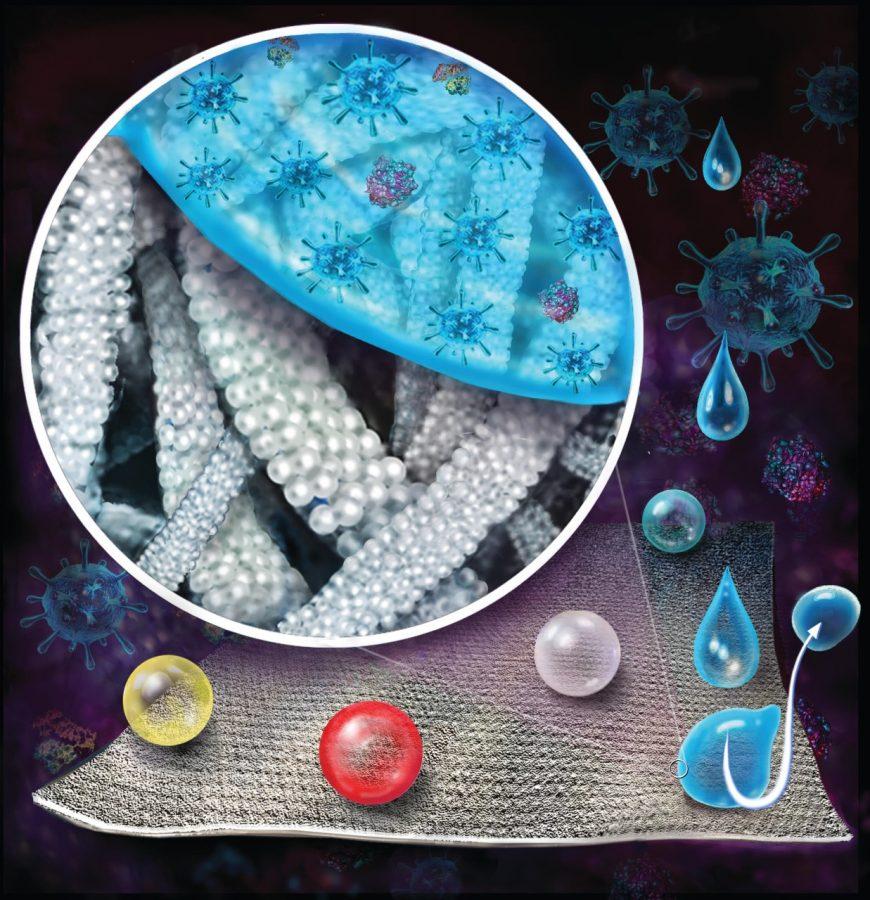
Courtesy of Swanson School of Engineering
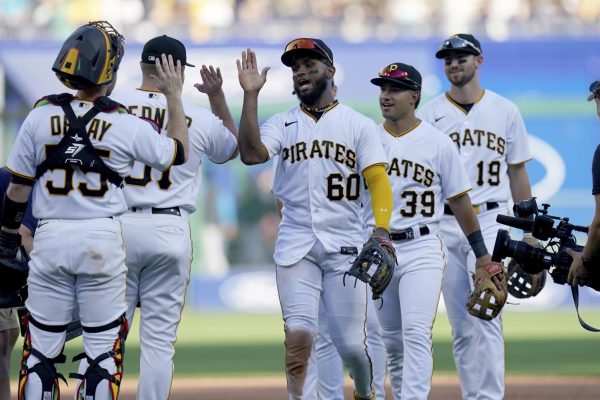
An illustration demonstrates the fluid repellent quality of treated textiles.
May 19, 2020
A shortage of personal protective equipment for hospital employees and volunteers during the COVID-19 pandemic has created challenges for the U.S. health care system, while at the same time posing a great danger in the transmission of disease.
Researchers at the Swanson School of Engineering’s Laboratory for Advanced Materials at Pittsburgh and the Ophthalmology Department’s Charles T. Campbell Lab are collaborating to create virus-repellent textiles for medical professional use.
The initial research effort, funded by the Department of Industrial Engineering, began last summer to create reusable textiles that are mechanically durable and resistant to various viruses, such as those that cause conjunctivitis and acute respiratory disease. But due to the COVID-19 pandemic, the researchers are now pivoting to work on SARS-CoV-2, the virus that causes COVID-19.
The team is currently trying to connect with manufacturers to develop full-scale prototypes, as well as obtain additional research grants. As a result of the pandemic, the timeline of activity has halted.
Paul Leu, an associate professor of industrial engineering, and Anthony Galante, a graduate student, noticed that their reusable textiles were resistant to proteins, blood and bacteria.
Eric Romanowski, the research director at the Campbell lab, said he and Robert Shanks, the director of basic research in the Department of Ophthalmology realized that certain viruses would likely have the same repelling effects due to their protein-coated structure.
“We used different types of adenoviruses that cause both respiratory infections and conjunctivitis,” Romanowski said. “These viruses are surrounded by proteins, and so if the material was already repelling proteins, it would also repel viruses. This turned out to be the case.”
But researchers noticed a key difference in the outer layer of some viruses versus others, creating an issue when developing textiles resistant to SARS-CoV-2. The adenoviruses that researchers had been using to test resistance are surrounded by a capsid, or protein shell, while envelope viruses such as SARS-CoV-2 have a lipid envelope surrounding their capsid that affects binding.
“Our material prevents protein-binding,” Shanks said. “Because proteins are essential to virus binding, I am optimistic that we will be successful. However, there is the caveat that the lipid envelope interaction with the textile could present problems.”
Galante led the experimental process to create virus-resistant textiles using a piece of nonwoven polypropylene microfiber cloth, the most common material used in lab coats and other medical supplies.
The cloth’s coating is created in two steps. First, using a syringe, Galante created a layer of polytetrafluoroethylene nanoparticles on the cloth’s exterior. A heat treatment then fuses the nanoparticles to the cloth surface, creating the coating. After extensive durability tests, the coated textiles maintained their virus-, liquid- and protein-repellent properties. To gauge virus-resistant properties of the textiles, a test must be performed to count plaque-forming units, or the number of potent virus cells per unit of volume.
“We take the amount of liquid present on the textile surface and inject it into human lung cells after a period of incubation time,” Galante said. “After two weeks, we stain the cells to identify plaques, or infection sites, which are then counted.”
The researchers have yet to test the textile’s durability in an autoclave, a machine that health care providers often use to apply heat to personal protective equipment and prevent the spread of infection. The textiles should last for 50 wash cycles, the standard for reusable protective equipment. Thus far, the researchers have tested the material with only 12 wash cycles. Leu estimated that personal protective equipment made from their reusable textiles will save hospitals money in the long run, in comparison to disposable equipment.
“Because it’s being incorporated into reusable medical textiles, we think that on a per cost usage basis, it should save a substantial amount of money,” Leu said. “We’re talking about something that can be used over 50 times versus something that can be used only once.”