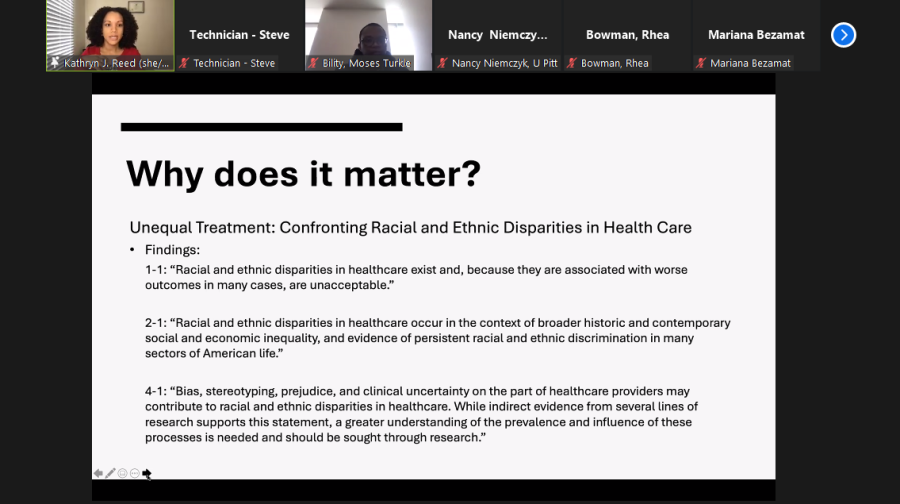
Lecture highlights racial disparities, prejudice within the medical field
Kathryn Reed, the vice chair for equity, inclusion and community engagement and assistant professor of PA studies at the School of Health and Rehabilitation Sciences, presents at Thursday’s installment of the Race & … Lecture Series on Zoom.
January 28, 2022
When Serena Williams gave birth to her daughter in 2017, she informed her health care providers of her history of clotting disorders and that she was struggling to breathe post-delivery.
Despite this, her providers initially dismissed her needs. She was eventually rushed into emergency surgery and bedridden for six weeks after her delivery. Kathryn Reed, the vice chair for equity, inclusion and community engagement and assistant professor of physician assistant studies at the School of Health and Rehabilitation Sciences, said Williams’ experience is not uncommon for Black women and other minorities, and is a result of racial bias within healthcare.
“If it’s happening to her then we can almost conclusively say that it’s happening to lots and lots of patients outside of that purview,” Reed said.
Reed presented Thursday on Zoom and in person at the “Race & … Lecture Series.” The series is a part of the “Race and Social Determinants of Equity, Health and Well-being Cluster Hire Initiative,” which Ann Cudd, provost and senior vice chancellor, and Anantha Shekhar, senior vice chancellor for health sciences, launched in 2020.
The lecture highlighted the underrepresentation of minorities in the healthcare system as well as racial and socioeconomic disparities in fetal mortality rates.
Reed said the quality of healthcare is significantly worse for racial and ethnic minority populations because of historic and current social and economic inequities, as well as bias, stereotyping and prejudice from health care providers. Reed said more diversity training for providers and representation of minority groups, specifically among PAs, is necessary to improve conditions.
“These beliefs, of course, were started during times when Black folks were enslaved in this country. And so the fact that it’s perseverating to now is very, very clear that we’re not in a post-racial society,” Reed said. “And also very, very clear that we need to be doing a better job of educating our students and having them unlearn some of these things before they start caring for us, right or for our families and people that we love.”
Reed said it is crucial for institutions like Pitt to create opportunities and spaces that allow for students who are typically underrepresented in medicine to enter the medical field.
“We need to be doing a better job of both bringing in students who are more diverse, graduating them ensuring their success, so they can show up and be healthcare providers for folks like Serena.”
Underrepresented in medicine, or URiM, is a term used by the American Medical Association to refer to racial and ethnic populations that are significantly underrepresented in the medical field compared to the general population, specifically Black, Latinx and Native American populations, according to Reed.
The National Commission on Certification of PAs’ 2020 Statistical Profile found that Black, Latinx and Native Americans were significantly underrepresented among physician assistants compared to the general makeup of these groups within the U.S. population. Reed said several barriers specific to Black and brown communities, including lack of exposure to the PA profession early on, the cost of PA education, the admissions processes and a lack of access to support in the PA education and career processes lead to this underrepresentation.
Dr. Onome Oghifobibi, an assistant professor at the School of Medicine’s Department of Pediatrics, highlighted statistics within Allegheny County and the United States regarding infant mortality and premature birth.
He said the infant mortality rate in the United States was 5.6 per 1000 live births in 2020, which is “pretty low,” but there are still high rates in different areas of the country, especially among Black women. He also noted that the leading causes of infant mortality are premature births, low birth weight, congenital anomalies and trauma.
“Infant mortality represents the overall health and well-being of our community and it reflects the maternal living and working conditions and social environmental conditions in which people are born, live, work and age,” Oghifobibi said.
Oghifobibi said Allegheny County is one of the areas that displays high infant mortality and premature birth rates, with significant racial disparities. According to March of Dimes, from 2017 to 2019, premature births in Black infants was almost twice as high as other races in Allegheny County, and this rate was worse than the national average.
“Unfortunately, I think the infant outcomes in our county are complex and the reasons why are essentially deeply rooted in the historical context of the city and state in terms of segregation, racism and distribution of resources,” Oghifobibi said.“Now if we look at the causes of infant mortality, like I said, prematurity movements, there’s also significant racial differences.”
According to Oghifobibi, the Federal Infant Mortality Review Program, the Federal Maternal and Child Health Bureau and the U.S. Health Resource and Service Administration aim to tackle infant mortality by evaluating the social, economic and cultural factors associated with these deaths.
“The goal of FIMR is to reduce fetal, neonatal and infant deaths by improving the community resources and service delivery systems,” Oghifobibi said. “It comprises of interdisciplinary groups of professionals and community leaders.”
Over the past two years, Oghifobibi and others worked to establish the FIMR program in Allegheny County by collecting data and engaging with community members. He said they established a committee for this program which plans to meet starting next month, and will evaluate morality rates as of January 2022.
He said the presence of several health care systems within the area such as UPMC, Allegheny Health Network, Heritage Valley Health System, St. Clair Health and the Midwife Center made this process easier.
“So we have a lot of people who care for women and children in the community and we’re trying to bring everybody to the table and have a conversation about looking at the problems and issues and trying to come up with solutions,” Oghifobibi said.
A previous version of this story referred to Oghifobibi as a neonatal medicine fellow. Oghifobibi is an assistant professor. It also referred to the infant mortality rate in the United States as 5.6%. It is 5.6 per 1,000 live births. The article has been updated to reflect these changes. The Pitt News regrets these errors.