Opinion | It’s okay to hate your birth control options — even right now
July 18, 2022
Hormonal birth control, or “the pill,” was something heavily suggested to me by my mom and my doctor virtually as soon as I became a budding teenager.
I had acne and a boyfriend, so there was good reason to start taking a contraceptive. It did everything it should have — cleared up my skin and prevented me from getting pregnant. But, the side effects were often unbearable — and seldom talked about.
Every time I received a birth control package it came with a giant sheet of paper listing all of the risks and concerns to consider. Unsurprisingly, this went straight into the trash because realistically, what were my other options? Getting pregnant while I was still a child myself?
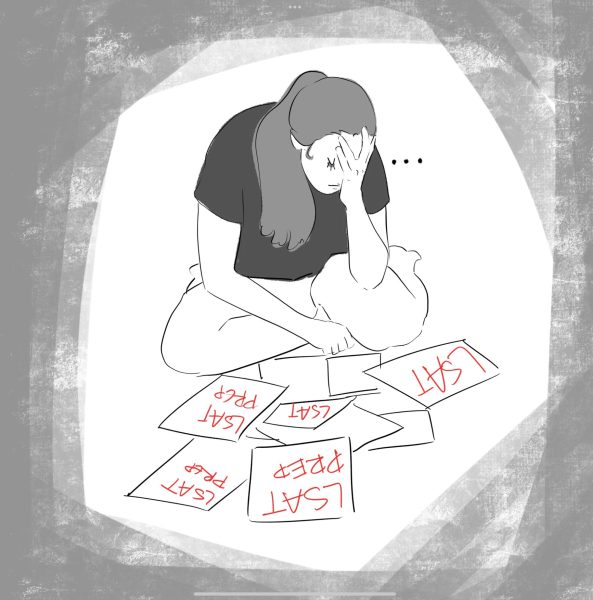
Just about three weeks ago, the Supreme Court voted to overturn Roe v. Wade. Considering that I’m not on any form of hormonal birth control or IUD, I’m susceptible to pregnancy.
Although I live in Pennsylvania, where abortion rights are currently intact — yet remain uncertain with the 2022 governer’s race — my bodily autonomy shouldn’t be politicized because of what birth control method I decide to use.
The right to an abortion is a human right, point blank. So is the right to choose what birth control methods I feel are appropriate for me and my partner. Frankly, I don’t think there are enough desirable options for people with uteruses, and even less feasible options for those without one.
There are various birth control options for people with uteruses, most of which are hormonal. These methods contain estrogen and progestin, which are continuously released into a person’s bloodstream through either a patch, pill, implant, ring or shot. Each hormone already occurs naturally, but on birth control they’re released in higher concentrations so the ovulation cycle stops. These hormones already create uncomfortable and undesirable, yet normal, symptoms on a monthly cycle, causing premenstrual syndrome (PMS) symptoms such as mood swings and cramping.
As one might expect, higher levels of these hormones cause the same symptoms, as well as weight gain and low libido in some patients. There are some other, much more serious, side effects of hormonal birth control, including blood clots, certain cancers and depression. Even if some of these side effects are rare, hormonal birth control can make everyday life very difficult, understandably making it a less desirable option for some people.
In addition, different brands will likely make you feel differently. But hormonal birth control shouldn’t be the only option keeping me from getting pregnant.
The patch, the pill and the ring aren’t going to hurt, but they each come with their own drawbacks. Their efficacy rates are around 91%. The implant and the shot will cause you some temporary pain — though not as much as labor and delivery. Their efficacy rates are 99% with perfect use, but 94% with the shot, as some people forget to schedule their appointments on time. Both the shot and the implant require an appointment with a doctor. The shot lasts about three months, until the next appointment, while the implant lasts about three years. If you aren’t fond of needles, though, then these choices probably aren’t the best options for you.
Then comes the IUD. Their efficacy rate is over 99%. There are both hormonal and copper IUDs, but regardless, both change how sperm move to prevent them from getting to the egg. The copper IUD lasts for around 12 years and the hormonal IUDs last for an average of five years. This might seem like a good option, but IUD insertion can be painful. But if you’re looking for something long-term and nonhormonal, this could be one of your only solid options.
Tubal ligations and vasectomies are also options, vasectomies being much less invasive than the former. Their efficacy rates are over 99%. These procedures are permanent, but can be reversed later on if need be. It is unlikely that these options will be performed on young people, being that some doctors believe that patients or their partners will regret them later on. Doctors will often try to deter their patients from these procedures, instead giving them, like in this example, information on other birth control options.
Of course, there are still over-the-counter birth control methods that are available to everyone with the means to purchase them. These include condoms, spermicide and emergency contraception. Condoms are around 85% effective, spermicide is 72% effective and emergency contraception is anywhere from 75-89% effective. However, emergency contraceptives are not accessible to everyone — Plan B has a weight limit of 155 pounds. The main problem with these options is that they aren’t long term, and thus leave people more susceptible to human error than the aforementioned long-term options.
Looking at all of these options, it is safe to say that there is a lot to choose from. However, no one choice is 100% perfect. If you want a birth control option without hormones, you’re severely limited in what’s left for you — especially if you’re the one with a uterus. If you want a birth control option without hormones or pain, you’re practically left with just over-the-counter options which are less effective.
With that being said, all of these side effects are arguably better than having a child when you aren’t ready. We have more options than we did in the past, but we should have even more options in the future.
Although long-term birth control options for people with penises have shown promise as of recent, there are still very few options available solely for them. Birth control is inherently a uterus owner’s issue, presumably because they can get pregnant, but it doesn’t have to be this way. After all, it takes two.
I think that birth control should be more than just a uterus owner’s issue, though. It is time to put more funding and research into the pursuit of male birth control so that all sexes can equally carry the responsibility of not wanting a child at the time.
In the same instance, it shouldn’t be a uterus owner’s responsibility to immediately go on long-term, hormone-altering birth control as soon as they hit puberty so that their partner can have a sex life free of care and worry. If you don’t want to be on long-term birth control, you don’t have to be, and you shouldn’t feel pressured to just because you have the potential to carry a child.
“My body, my choice” doesn’t just simply pertain to abortion. It outlines that what people with uteruses do with their body is completely up to them, and that their uterus is no one else’s property.
Jessica Snyder primarily writes about controversy in art and politics. Write to her at [email protected].