The Pitt Prescription | The invisible work of pharmacists: What really goes on behind the counter
The Pitt Prescription is a biweekly blog where student pharmacist and senior staff writer Elizabeth Donnelly provides tips on how to stay healthy in college. This edition was reviewed by Karen Pater, PharmD., CDCES, BCACP.
April 20, 2023
Pharmacists are the most accessible healthcare providers — data shows that patients see community pharmacists nearly twice as often as any other qualified health professional.
Although studies reveal that the majority of patients view pharmacists as integral members of the healthcare team, many members of the general public lack the basic understanding of what a pharmacist does. I’ve seen both ends of the spectrum.
As a student pharmacist, I’ve evaluated patients who will only listen to medical advice from pharmacists and will take my word as law, but I have also had instances where I’ve been called a “glorified pill counter” and told to “stay in my lane” when attempting to provide patient education. Most people, I’ve found, fall in the middle of these two extremes. While they recognize that pharmacists are knowledgeable healthcare workers, they don’t understand the intricacies that go into our daily responsibilities.
In the US, pharmacists are required to complete doctorate-level training in order to practice pharmacy. Similar to how physicians earn their doctor of medicine (MD) or doctor of osteopathic edicine (DO) degree, pharmacists earn a doctor of pharmacy (PharmD) degree. However, the degree doesn’t make an individual a pharmacist — there are still two exams required in order for someone to legally practice pharmacy. These exams are the pharmacy licensing exam, known as the NAPLEX, and the pharmacy law exam, which differs from state to state. Once an individual successfully passes these exams, they earn the title of registered pharmacist (RPh).
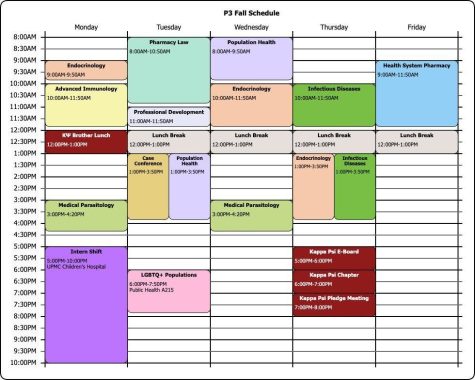
The PharmD curriculum at Pitt is incredibly rigorous at times, with coursework made up of biomedical sciences (e.g., medicinal chemistry, pharmacokinetics), therapeutics (e.g., cardiology, oncology) and experiential learning via both introductory and advanced clinical rotations. During the four years of graduate education, student pharmacists develop intricate drug knowledge that most other healthcare providers do not have.
There are many fields a pharmacist may pursue using this knowledge of medications. A slight majority (approximately 58%) of pharmacists work in community pharmacies (you may also hear them referred to as “retail” pharmacies) like Walgreens or Rite Aid. The remainder work in a myriad of different fields, including ambulatory care, hospital pharmacy and the pharmaceutical industry, to name a few.
Pharmacists may also pursue post-graduate training through residency programs similar to that of physicians or through fellowships. While not mandatory, many pharmacists complete further training to become clinical specialists in the pharmaceutical field of their choosing. This additional training continues to strengthen the PharmD curriculum and helps pharmacists become experts in niche fields of pharmacy.
Given the complexity of the field and the many different roles and responsibilities that pharmacists can undertake, it would be impossible to discuss all of them in a concise manner. Since the majority of pharmacists practice in the community setting, and since that is where you will have the most opportunities to interact with a pharmacist, community pharmacy will be the focus of the remainder of this article.
Community pharmacists play a vital role within the U.S. healthcare system by helping patients manage their medications and providing expert counseling on therapeutic regimens. Not only are they responsible for dispensing physician-prescribed medications, but they are also in charge of ensuring the prescribed medication is appropriate for each individual patient. This means they must check the dose, frequency, active ingredients and more for all prescriptions. Thus, when a prescription is sent to the pharmacy, there is a lot more that goes into filling it than just printing out a label and pouring some pills into a bottle.
Community pharmacists review each patient’s medication history as well as any contraindications that are present. Contraindications refer to situations where a medication or treatment should not be used due to the potential for harm or adverse effects. In other words, a contraindication means that the medication prescribed is inappropriate to use on that patient. Pharmacists often catch inappropriate prescriptions before they are dispensed to the patient. Many times, pharmacists catch prescription errors and contact the prescribers to correct it without the patient ever knowing there was an issue in the first place.

Community pharmacists also work closely with insurance companies to try and ensure proper coverage of medications and to find alternative therapeutic options if the original prescription medication is not covered. In addition to the clinical review of prescriptions, community pharmacists are also responsible for providing several immunizations like the flu shot, performing comprehensive medication reviews and counseling patients on any new medications if questions arise. Most of this work is done behind the scenes, so patients often don’t see it going on.
Community pharmacists also often offer monitoring services to ensure that medications are producing the desired clinical outcomes. These services may include blood pressure monitoring, diabetes care services, cholesterol monitoring or test and treat services and point of care testing, such as the nasal swabbing performed at many pharmacies to test for COVID-19.
There were times where I was on hold with an insurance plan for over an hour while I worked to enter new prescriptions and verify their appropriateness while also fielding questions about over-the-counter medications and addressing patients who were upset due to the ongoing drug shortages. Community pharmacists deserve credit for the work they do, and I commend them for all of their patient care efforts.
The field of pharmacy offers such a wide range of career paths for individuals entering the profession. While I have discussed community pharmacy, the most common pathway, there are so many other vital ways in which pharmacists act as integral members of the healthcare team. Pharmacists are the medication experts, and they play a critical, yet often overlooked, role in ensuring patients receive safe and effective medication therapy.

Note from the writer: I will be graduating as a Doctor of Pharmacy one week from today, on April 28, 2023, and I’m excited to be completing post-graduate training as an ambulatory care resident at a Veterans Affairs (VA) Hospital. There, I will be working as a member of the patient-centered care team and will play an active role in medication management, prescribing and counseling. Writing “The Pitt Prescription” for the last 4 years, and working for The Pitt News for the last 6, has been a rewarding experience and has helped me enhance my knowledge of medical communications (yet another field that many pharmacists pursue). I hope that these articles have helped you better understand the intricacies of pharmacy and self-care. And remember, if you’re ever unsure about anything related to medications, your local pharmacist is equipped with the knowledge to help.
This is Elizabeth’s final piece with The Pitt News. She started writing for The Pitt News her first year of college in 2017 and her writing has primarily focused on self-care and pharmacological topics.