Opinion | Birth control access is still a problem — even in 2023
June 27, 2023
Birth control is not something that we, as individuals who experience a period, want to take. For many of us, it is out of a necessity — whether that be to prevent pregnancy, make our periods more manageable or help prevent or lessen symptoms of acne, endometrial and ovarian cancers, menstrual cramps, cysts, infections, anemia and other health concerns.
There are now various types of birth control — the standard birth control pill, Nexplanon arm implant, intrauterine device (IUD), a shot and an arm patch, among other options. There are birth control options now appearing for men — however, they are relatively new and still widely debated.
Birth control has changed since its initial creation and is now, finally, less stigmatized in society. However, unfortunately this does not mean it is easy for individuals who have a menstrual cycle to get access to birth control.
Currently, I have been trying to get an answer as to whether my insurance will cover the Nexplanon implant for almost two months. My insurance company only covers the birth control shot and pill, so I had to have my medical provider submit a form to try to get the implant covered by my insurance. For my insurance to cover this, they are requiring that my medical provider submit clinical information to prove medical necessity. My insurance will cover the cost of the procedure but not the cost of the implant without seeing the necessity of doing so.
Access and coverage of birth control does vary depending on someone’s insurance — however, after listening to my friends’ similar experiences to my own, it appears that this is a major issue in American society. Proving that birth control is medically necessary can be difficult as everyone’s menstrual cycle affects them in different ways and may not always be considered as a medical necessity.
More than 19 million women live in contraceptive deserts in America, which are areas lacking access to a full range of birth control methods. Among the individuals living in a contraceptive desert, about 1.2 million of them also live in counties without any health centers that have full birth control services.
Data from Advocates for Youth shows that the majority of young people across the country face barriers to accessing birth control that leads to delayed doses, side effects and an inability to use contraception. Of the individuals from the 42 states surveyed, an overwhelming majority of 88% indicate that they struggled to access birth control, and 55% experienced multitudes of barriers that prevented them from starting birth control on their preferred timeline.
Of the 55%, 58% had a pregnancy scare, 20% got pregnant and 16% had abortions. “For young people — particularly low-income, POC, trans, queer and other marginalized youth — accessing birth control can be unnecessarily difficult but crucially important to preventing unplanned pregnancies and protecting bodily autonomy,” according to Advocates for Youth.
Access to affordable health care is not available throughout the entirety of the United States. Gaps in equal and equitable ways of receiving birth control affect overall health outcomes for individuals. Being able to have access to birth control is important for public health, especially taking into consideration that almost 50% of pregnancies in America are not planned.
Common barriers to receiving birth control include:
- Racial and ethnic bias
Individuals of color face structural and societal issues affecting their ability to access effective birth control. Hispanic and Black women have the highest rates of unintended pregnancy, and statistically, birth control usage in Black women ages 15-49 is lower compared to white women. Factors playing into these statistics can include low income, lack of insurance or no health insurance and a lack of information to learn about contraception.
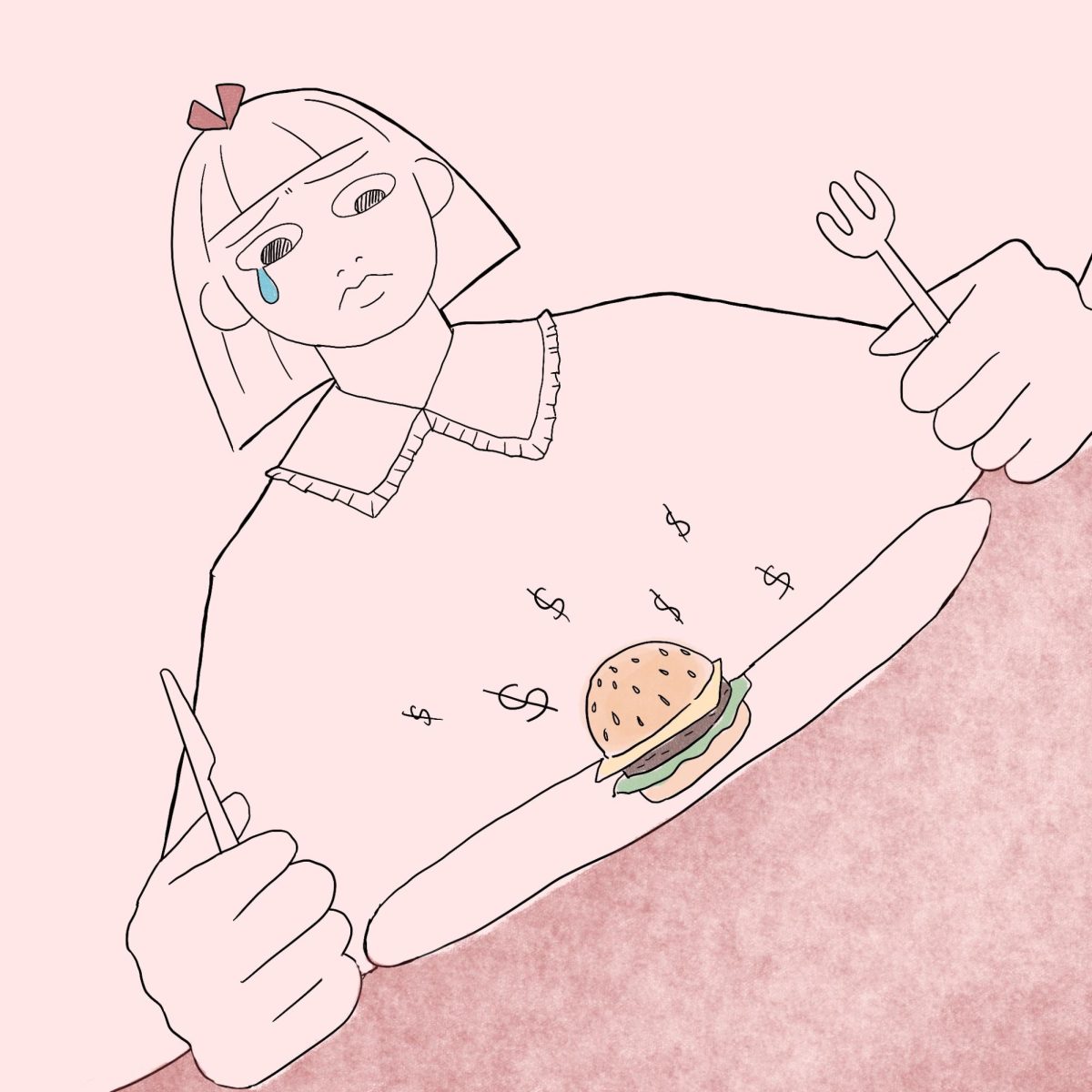
- Cost of birth control
For most birth control options you need a prescription from your medical provider. The overall cost of time and money prohibits women from receiving birth control. The upfront costs of long-acting reversible contraceptive, LARC, methods is very high and may be out of reach for those without health insurance coverage. A total bill for an IUD can cost more than $1,000. Even if you have private health insurance, out-of-pocket costs, deductibles and copays can limit your access, even if your insurance already covers it in the first place.
- Location
There are a growing number of contraceptive deserts and areas lacking funding from federal and state programs, and, especially since Roe v. Wade was overturned, state-level politics influences how funds are used. If you live in a contraceptive desert and can not easily drive out of these boundaries, this creates additional barriers to access.
- Lack of awareness
Some individuals believe that birth control is the same as abortion — this is not the case. In sex education, many youth hear abstinence-only curriculums, which creates an incorrect idea of the effectiveness of contraceptives and worries about safety and side effects of birth control. More comprehensive sex education is necessary to form a better understanding of sexual health and birth control services.
- Other barriers to birth control
Religious beliefs or moral attitudes keep an individual from receiving the birth control or family planning that works for them. Many large health systems throughout the country are funded by religious organizations, and the core beliefs of these organizations can create roadblocks and legal hurdles when you ask your healthcare provider for a birth control or contraceptive prescription. Six states legally allow pharmacists to refuse to fill your prescription or give you emergency contraceptives where alternative options are not always available.
About half of women who tried to receive a prescription for hormonal contraception report problems obtaining their prescriptions or refills. Additionally, uninsured and Spanish-speaking women are significantly more likely to report difficulties. With the given improvements society has made to the effectiveness of birth control, the fact that unintended pregnancies threaten public health is most likely attributed to the lack of access to birth control.
Birth control is something I would love to not have to worry or constantly think about, and I would reckon is the same consensus for most of those who need it. Having access to birth control is necessary for people to live their lives freely, safely and without discomfort.
Although it may not be easily understood as to why birth control is medically necessary, think about it from the perspective of an individual who experiences a menstrual cycle. Explain that to someone who can barely get out of bed to go to work because of their period symptoms or to someone whose life is altered for a week or more every month because of something that could be managed by medication.
Emily O’Neil writes primarily about societal issues, politics and campus life. Write to her at [email protected].